Immunoglobulin replacement therapy decreases the risk of infection in haematological malignancies
A systematic review and meta-analysis of immunoglobulin prophylaxis in chronic lymphocytic leukaemia (CLL) and multiple myeloma (MM) finds that infusions of immunoglobulin (IgG) can reduce the risk of major infection and infection frequency, despite not having an effect on mortality. Immunoglobulin therapy is well-tolerated and can be used based on evidence-based guidelines.
Rapid development of new therapies targeting B-cell signaling and survival pathways and increased use of chimeric antigen receptor T-cell (CAR T) therapy will likely result in more acquired deficiencies of humoral immunity and infections in persons with cancer.
Treatment with IVIg should be considered in patients with SID who suffer from severe or recurrent infections, ineffective antimicrobial treatment and either proven specific antibody failure (PSAF) or serum IgG level of <4 g/l.
- Raanani, P. et al., Leuk Lymphoma, 2009; 50:764
- Debes, A. et al., Pharmacoepidemiol Drug Saf. 2007;16:1038
- Ueda, M. et al., Blood Reviews 2018; 32:106-115
- EMA. Guideline on core SmPC for human normal immunoglobulin for intravenous administration (IVIg) 2016
Immunoglobulin replacement therapy decreases the risk of infection in CLL and MM


Results of a systematic review of the efficacy of IgRT in secondary immunodeficiency in CLL and MM from
3 clinical trials showed a significant reduction in the relative risk of major infections with IgRT. The absolute risk reduction was 19%.


The relative risk of clinically documented infections in CLL and MM was reduced by 51% with IgRT vs placebo or no treatment.
- IgRT: immunoglobulin replacement therapy
- Raanani, P. et al., Leuk Lymphoma, 2009; 50:764
Immunoglobulin replacement therapy decreases the risk of infection in haematological malignancies


Results of a non-interventional study suggest that the use of intravenous and subcutaneous immunoglobulin replacement therapy reduces the risk, frequency and severity of infections in haematological malignancies associated with secondary immune deficiency.
The overall annual incidence of infections decreased by 22% with immunoglobulin replacement therapy compared to before treatment. Furthermore, significantly fewer infections requiring antibiotics and infections that led to hospitalisation were reported during Ig replacement therapy.
- IgRT: immunoglobulin replacement therapy
- Benbrahim, O. et. al., Hematology 2018; 24(1):173-182
Immunoglobulin replacement therapy decreased the risk of infection in MM associated with hypogammaglobulinaemia


Immunoglobulin replacement therapy (IgRT, Arm-A), compared to control without IgRT (Arm-B), significantly reduced
- the number of infections (A, B)
- the number of days
of hospitalisation/year (C) - the number of days
of antibiotic use/year (D)
By reducing the rate of infections, prophylactic administration of subcutaneous immunoglobulin
- might improve adherence to chemotherapy and health-related quality of life
- is potentially cost-effective in reducing the need for hospitalisation and the use of antibiotics
- Adapted from Vacca, A. et al., Clin Immunol. 2018; 191:110-115
IgRT decreased cytomegalovirus and acute graft-versus-host disease following haematopoietic stem cell transplantation


Immunoglobulin prophylaxis significantly decreased the risk of acute GVHD and CMV diseases
Relative risk of CMV disease decreased by 48% (2 studies, n=167) and acute GVHD decreased by 22% (8 studies, n=1097) with prophylactic use of immunoglobulin replacement therapy.
This study was a systematic review and meta‐analysis of randomised controlled trials that assessed clinical outcomes of immunoglobulin prophylaxis versus placebo in haematopoietic stem cell transplant recipients.
- IgRT: Immunoglobulin replacement therapy, CMV: Cytomegalovirus, GVHD: Graft vs. host disease
- Ahn, H. et al., Transfusion 2018; 58(10):2437-2452
As cancer therapies become increasingly personalised, decisions about immunoglobulin replacement therapy need to be tailored to the individual
Parallel to personalised cancer therapies, the decision to give immunoglobulin replacement therapy is best individualised
Factors to take into consideration: 1. Disease, 2. Therapy, 3. Prior infections, 4. Serum antibody titers, 5. Ability to respond to anti-infective vaccines
- Ueda, M. et al., Blood Reviews 2018; 32:106-115
Immunoglobulin therapy is very well-tolerated in SID


95% of 2'409 patients reported no adverse drug reactions when treated with intravenous immunoglobulin (IVIg)
Secondary immune deficiency in these patients was due to chronic lymphocytic leukaemia (728), multiple myeloma (339), bone marrow transplantation (566), other causes (776).
In this 10-year observational study, IVIg was very well tolerated in routine clinical use.
- Only 5% of 2’409 patients experienced adverse drug reactions
- Only 0.62% of 20’642 infusions were associated with adverse drug reactions
- IVIg: intravenous immunoglobulin
- Debes, A. et al., Pharmacoepidemiol Drug Saf. 2007; 16:1038
Immunoglobulin therapy can be administered intravenously or subcutaneously


Immunoglobulins can be administered via IV or SC routes, with similar efficacy and safety
- The dose should be adjusted individually to maintain IgG levels ≥5 g/L
- Patient preference may be a key consideration when deciding on the administration route
- Figure adapted from: Jolles S. et al. Clin Exp Immunol 2015. 179:146
- Agostini, C. et al., Expert Rev Clin Immunol. 2016; 12:921
- Kerr, J. et al., Int J Infect Dis. 2014; 5:629
- Spadaro, G. et al., Clin Immunol. 2016; 166-7:103
- Windegger, T. M. et al., Transfus Med Rev. 2017; 31:45
Current clinical practice in the management of secondary immunodeficiency in haematological malignancies
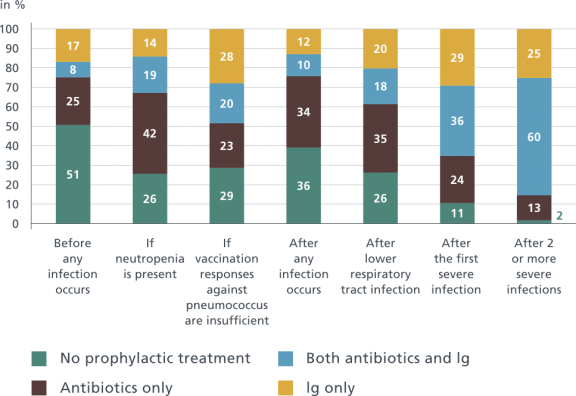

An international online survey of 230 physicians responsible for the diagnosis of SID and the prescription of IgRT in patients with haematological malignancies was conducted.
Serum immunoglobulin was measured in 83% of patients with multiple myeloma, 76% of patients with chronic lymphocytic leukaemia, and 69% of patients with non‐Hodgkin lymphoma.
Most physicians (85%) prescribed Immunoglobulin replacement therapy after ≥2 severe infections.
In Italy, Germany, Spain, and the United States, immunoglobulin use was above average in patients with hypogammaglobulinaemia, while in the UK considerably fewer patients received IgRT.
The use of subcutaneous immunoglobulin was highest in France (34%).
- Ig: immunoglobulin
- Adapted from Na et al., Eur J. Haematol. 2019; 102:447–456. Sample size: (USA [N = 50], Canada, UK, France, Italy, Spain, Germany [N = 30 each]
Guidelines for the use of immunoglobulin replacement therapy in haematological malignancies and HSCT*
EMA guidelines for human normal immunoglobulin core SmPC (released in 2018)
“Replacement therapy in adults, and children and adolescents (0-18 years) in […] Secondary immunodeficiencies (SID) in patients who suffer from severe or recurrent infections, ineffective antimicrobial treatment and either proven specific antibody failure (PSAF) or serum IgG level of <4 g/l.”
2017 Work Group Report of the American Academy of Allergy, Asthma & Immunology
IgRT use is recommended in CLL patients with recurrent bacterial infections in presence of HGG and subprotective levels of specific antibody production following immunisation to diphtheria, tetanus or pneumococcal infection.
It is also recommended in MM patients with recurrent bacterial infections in presence of subprotective levels of specific antibody production following immunisation to diphtheria, tetanus or pneumococcal infection.
IgRT use may be considered for patients with chronic GVDH and recurrent serious bacterial infections with proven antibody production defect.
- *For further guidelines and details, download the presentation
- GVHD: graft vs. host disease, HSCT: haematopoietic stem cell transplantation, HGG: hypogammaglobulinaemia
- EMA. Guideline on core SmPC for human normal immunoglobulin for intravenous administration (IVIg) 2018
- Perez, E. et al., J Allergy Clin Immunol. 2017; 139:S1
When to initiate immunoglobulin replacement therapy (IgRT) in antibody deficiency: a practical approach
Hypogammaglobulinemia with infection


Jolles et al. developed their algorithm for decisions when the clinical situation is not clear, i.e. in the absence of a very low level of immunoglobulin production in association with an increased frequency of severe or recurrent infections.
- IgRT: immunoglobulin replacement therapy.
- Adapted from Jolles, S. et al., Clinical and Experimental Immunology 2016, 188: 333–341

